Monitor, Monitor And Monitor Some More
Once an intravenous infusion is initiated, monitor the infusion closely to ensure that it is infusing at the correct rate. If the fluids are infusing too fast, you will need to adjust the pump or roller clamp to slow the infusion down. If the fluids are infusing too slowly, first check the infusion site, looking for infiltration and if changing the position of the extremity changes the flow rate. Then open the roller clamp slightly to attempt to increase the infusion rate. If needed, re-position the extremity to an extended position, and flush the IV line with a 10 cc syringe filled with saline. Connect the syringe to the medication port, pinch off the tubing proximal to the syringe and gently push the saline into the IV line. Once the plunger depresses easily, withdraw the plunger slightly to draw up a small amount of blood, and insert the remaining fluid in the syringe. This signals that the line is patient again. Be sure to observe the IV site for any infiltration and pain. Discontinue infusion if the catheter appears to have dislodged from the vein.
During infusion, check the IV site for signs of infiltration and inflammation. How often you must check varies with the facility and often depends on what is being infused, so be sure to become familiar with your facility’s policies and follow them consistently each time you are caring for a patient who is receiving an IV infusion. Every time you inspect the site, take the opportunity to also check the time tape, solution, tubing, and flow rate.
To establish a baseline at the beginning of your shift, assess and document the condition of the IV site, solution, tubing, and flow rate. Ongoing assessments throughout your shift and at the end of your shift can be compared to what you assessed at that initial point.

Begin the assessment by inspecting the site for any redness or swelling. Next, gently palpate the area around the site and along the vein looking for any pain, firm tissue, or edema. Note the temperature of the skin near the site and along the vein, especially if you note any redness. Warm skin may indicate phlebitis.
Peripheral venous catheters are usually replaced every 72 to 96 hours, or according to your facility’s policy. Sometimes you may need to care for an IV line that was installed outside of your facility or during an emergency. In this case, be sure you are familiar with all of the components of the infusion and that there is no question about the sterility of the procedure used. Should you have any question about the sterility or patency of the IV, it may be best to install your own line. Do not disconnect a questionable but patent line before you have established another.
Patients with IV access are at risk for developing phlebitis and infiltration. Pediatric patients, patients with fragile veins, and patients who are receiving hypertonic, acidic or irritating fluids or medications are at an increased risk. More frequent and thorough assessment is recommended for these populations.
Signs and symptoms of phlebitis include pain, increased skin temperature, and redness along the vein. The degree of phlebitis is often documented on a scale from 0 (no symptoms) to 4 (most severe). Use the most severe sign or symptom to document your patient’s condition.
The most common treatment is to discontinue using the IV line and place a warm, moist compress over the affected area. It is recommended that a new line be established, especially in people who are “hard sticks”, before removing the original IV. Consult your facility’s policy to ensure correct treatment.
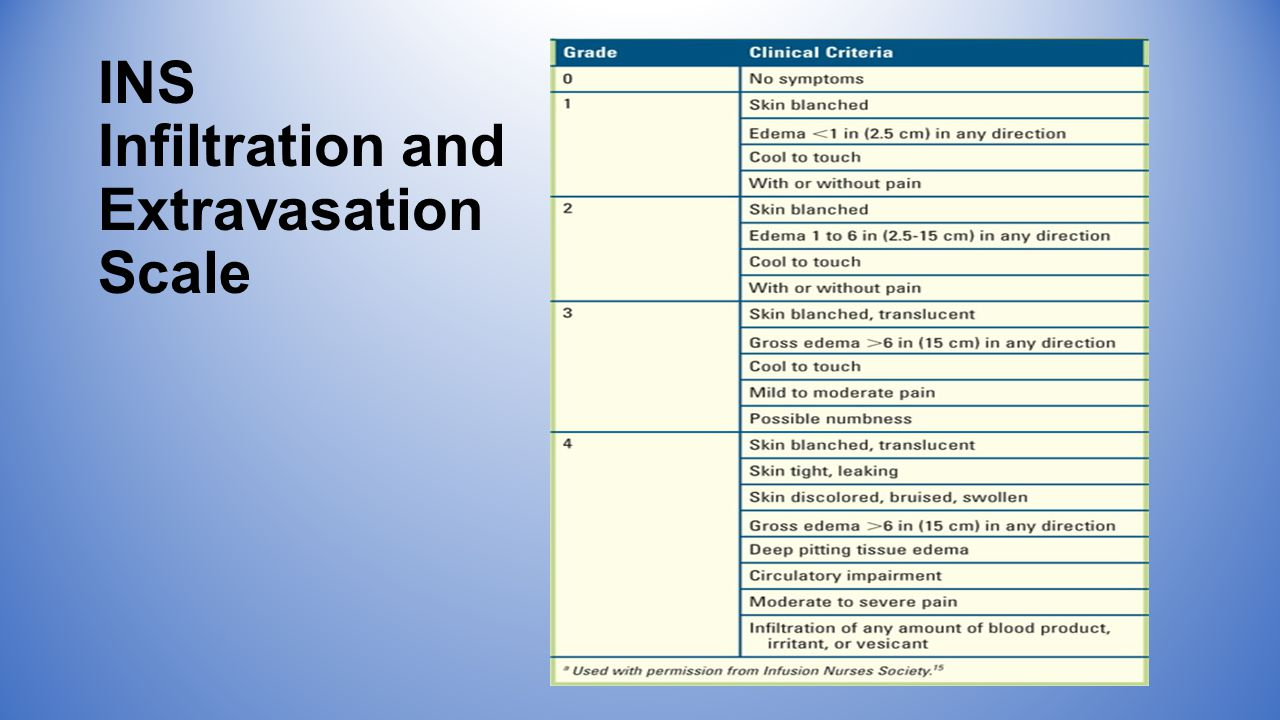
Infiltration results when the IV catheter is dislodged from the vein and fluid infuses into tissue. Signs and symptoms include localized edema, pallor, decreased skin temperature around the site, and pain. The degree of infiltration is documented on a scale similar to the one used for phlebitis. Again, document using the most severe sign or symptom.
The usual treatment is to discontinue the IV and elevate the extremity. A warm compress may also be placed at the site to help absorb fluid. Your facility may have specialized policies for treatment of infiltrations, especially if the infusion is caustic to soft tissues. Consult your facility’s policy for complete and correct treatment.
Extravasation is yet another complication of IV therapy. Extravasation is similar to infiltration, but is used specifically to indicate that medication has been infused into the tissues. Signs and symptoms include pain, stinging or burning at the site, localized edema, and redness.
Some medications can cause severe damage if infused into the tissue, not the vein, including necrosis. Therefore this complication should be treated quite seriously and quickly. Extravasation is documented on the same scale and in the same manner as infiltration.
Extravasation is usually treated by discontinuing the IV line and applying a cool compress to the area. If the medication has an antidote, orders for that antidote should be obtained and administered as soon as possible. Consult your facility’s policy for complete and correct treatment.